World Keratoconus Day
Happy World Keratoconus Day! It is the perfect opportunity to raise awareness about keratoconus (KC) and support patients and families living with this condition. In this article, the eye doctors at Rottman Eye Care discuss the significance of World Keratoconus Day, treatment options for KC, and answers to frequently asked questions about keratoconus.
What Is World Keratoconus Day?
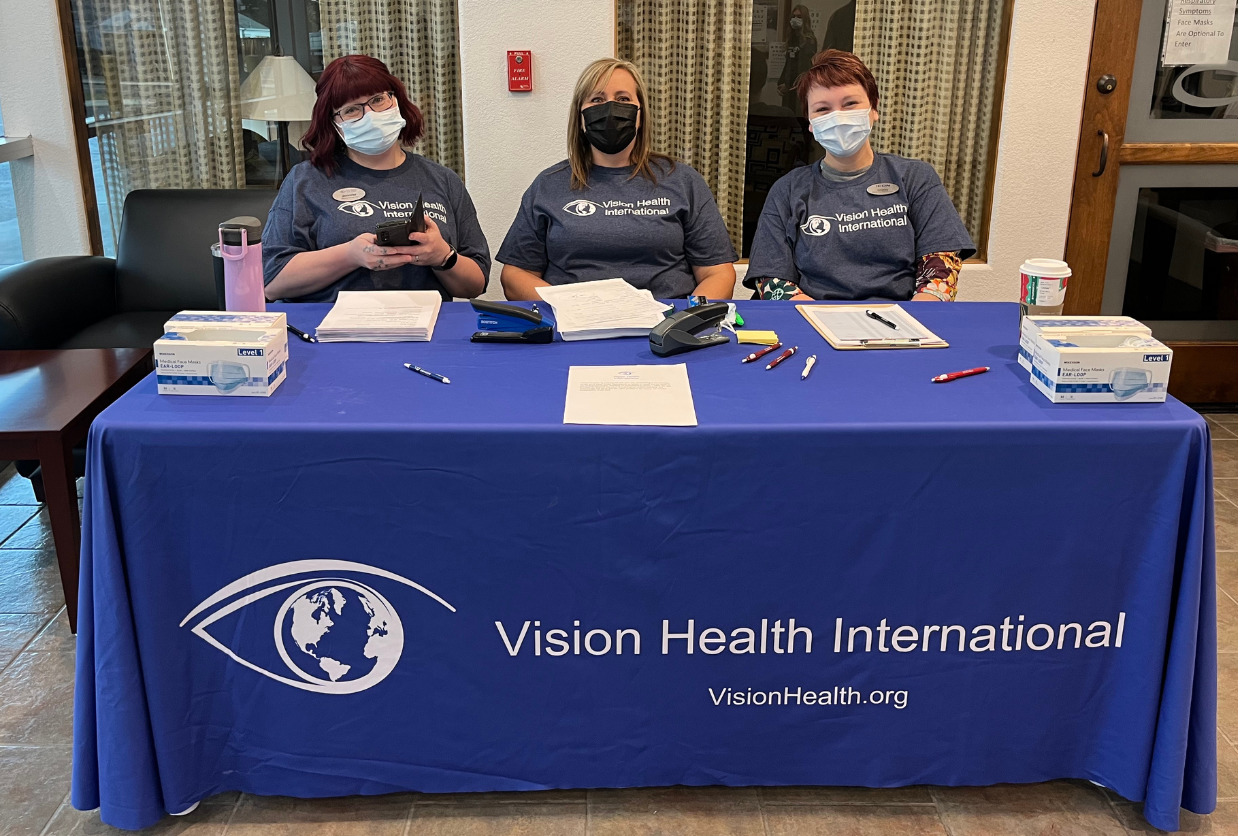
November 10th is “World Keratoconus Day,” used to raise awareness and provide support for those living with this sight-threatening disease. Rottman Eye Care is proud to celebrate the annual event, organized by the National Keratoconus Foundation (NKCF).
The foundation organizes many programs aimed at creating awareness about keratoconus. NKCF also funds several scientific research projects to investigate the causes and treatment of keratoconus. In addition, this day is aimed at educating the public about the impact of this condition on patients and their families and friends.
Many healthcare centers and hospitals organize webinars, community screening exercises, and seminars on World KC Day. The focus of these activities lies in scientific research to better understand the condition and its treatment options. It allows people to share their KC stories and partner with other organizations.
What is Keratoconus?
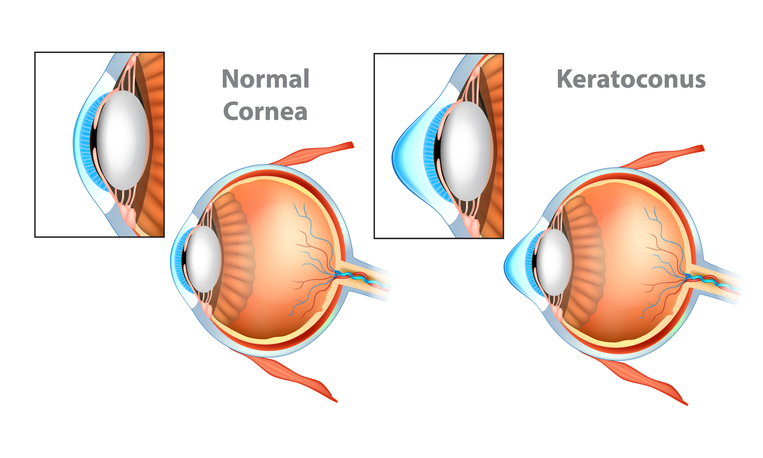
Normal Cornea and Keratoconus (KC) Cornea.
The term keratoconus originates from two Greek words– ‘kerato’ meaning cornea and ‘konus’ meaning cone. The cornea is a transparent, dome-shaped window in front of the eyes. It allows light to enter the eye and begins the process of focusing it.
Keratoconus is an eye condition in which the normally dome-shaped cornea gradually shrinks and declines to form a cone-like bulge. The change in the shape of the cornea brings light rays out of focus, leading to blurry, impaired vision, making activities like driving or reading difficult.
Keratoconus often affects both eyes. However, you may develop more severe symptoms in one eye versus the other. KC is linked to allergic conditions such as eczema, hay fever, and asthma. Patients often feel an itching sensation, causing them to rub their eyes, which can worsen the condition. There’s a strong genetic correlation, and many people with KC have a family history of the impairment.
Those with the following conditions may be more susceptible to developing KC:
- Down’s syndrome
- Retinitis pigmentosa
- Ehlers-Danlos syndrome
Symptoms of keratoconus may include:
- Distorted vision
- Amplified sensitivity to light
- Short-sightedness
- Astigmatism
- Constant changes of corrective lenses
- Eye swelling or redness
Book an appointment with us if your vision suddenly deteriorates and you show these symptoms. The KC specialist at Rottman Eye Care will examine the shape and curvature of your cornea using advanced equipment. You will receive recommendations specific to your case, taking your lifestyle into account.
How Common Is Keratoconus?
Less than 1% of the global population has keratoconus. However, 10% of those with keratoconus have parents with the condition. It affects both men and women, with some studies suggesting men are more likely to have it. The condition typically begins in early adolescence and continues developing into the mid-30s. Also, you are more likely to develop it if you have had refractive surgery in the past.
Treatment Options for Keratoconus

The two main objectives in the treatment of keratoconus are to reduce the disease progression of keratoconus and provide the best correction. Here are the best treatment options in managing the condition:
- Contact lenses designed for KC patients can enhance your vision.
- Corneal collagen crosslinking is an effective treatment for strengthening the cornea and stopping the further advancement of keratoconus. This minimally invasive procedure has been performed worldwide with outstanding results and works together with the following treatment.
- Ultraviolet light and eyedrop medication work to strengthen collagen linkage, producing a firmer cornea that doesn’t protrude outward. In addition, it may prevent the need for future corneal transplants.
- Corneal transplant may work for you if alternative non-invasive procedures and treatments fail to restore normal vision. Cornea transplant takes around an hour to perform in an outpatient setting. The surgical procedure involves the removal of the cornea, substituting it with a donor cornea. Corrective lenses ensure the best post-surgery results.
Your Rottman Eye Care professional will discuss all your options when you come in for an exam. We welcome your questions and will try to address all your concerns.
Contact Lens Options for Keratoconus
There are different contact lens options for keratoconus and the right one for you will depend mainly on the severity of your condition:
- Soft contact lenses can correct visual impairment during the initial stages of keratoconus. However, depending on how quickly the condition progresses, you may discover that your prescription needs to be adjusted regularly.
- Rigid gas permeable (RGP) or hard contact lenses: If you aren’t getting the correction you want using eyeglasses or soft contact lenses, consider RGP lenses. This may occur as keratoconus advances and your corneal shape becomes more irregular. These lenses form a smooth, light-refracting surface above the cornea to enhance vision. Rose-K contact lenses, a type of RGP, are designed to fit over an irregularly shaped eye far better than most other kinds of contact lenses. These lenses are created through a digital design process to give each patient a well-shaped lens. Rose-K lenses are the best option for treating corneal abnormalities, and patients at any stage can benefit from them.
- Hybrid contact lenses combine the durability and sharper vision correction of hard contact lenses with the convenience of soft contact lenses. Some individuals who struggle with wearing hard contact lenses find hybrid lenses more comfortable and easier to use. In addition, they like the clear vision possible with hybrid contact lenses.
- Scleral lenses are a great option for people with keratoconus. Scleral lenses are RGPs that are accurately measured to fit each eye. The gap between the corneal surface and the scleral lens is filled with a saline solution. This solution constantly hydrates and protects the cornea while correcting its imperfections. Scleral contact lenses often provide the best comfort and vision recovery option.
FAQs
How can keratoconus affect my life?
Keratoconus affects eyesight, which can lower the quality of life. Individuals living with the condition find it difficult to read, work, drive, and watch television. It can also lead to low self-esteem and reduce the ability to participate in recreational activities.
How common is keratoconus?
In the past, it was believed that about 1 in 2,000 individuals had this disease, but today, better detection methods indicate the number may be higher. Advances in technology and increased awareness allow more people to be properly diagnosed.
How do you measure the severity of keratoconus?
Our eye doctors can measure the severity of keratoconus by determining how thin the cornea is, its shape, and how steep the cones are.
Does keratoconus go away on its own?
No, keratoconus is a lifetime eye condition that does not go away on its own. In serious scenarios, a corneal implant might be necessary. Less severe keratoconus can be managed through the use of special contact lenses (soft, hard, scleral, hybrid). Scleral lenses are a special kind of contact lens that sit on the white part of the eye without resting on the cornea.
Can scleral lenses completely correct my vision?
Scleral lenses account for abnormalities that cause KC and may enhance vision better than other kinds of correction. However, you’ll need to wear eyeglasses over the lenses to see properly from any distance, especially if you’re over 40 and need reading glasses for work.
For how many hours can scleral lenses safely be worn daily?
You can wear scleral lenses for up to 12 to 15 hours daily. You need to remove the lenses, clean them, and apply sterile saline often to maintain the best possible vision and comfort.
How can I stop my keratoconus condition from getting worse?
Like any other disease, early detection is important in the treatment of keratoconus. If your keratoconus is progressing, you may need to have the corneal crosslinking treatment to halt the progression.
Keratoconus Treatment at Rottman
Our eye doctors, Dr. Randy Rottman and Dr. Ashely Ford, offer complete vision care at our Grand Junction eye care clinic. Dr. Ford specializes in the treatment of KC patients. We use advanced diagnostic technology and vision correction products and are committed to improving lives through better vision and outstanding patient experiences.
At Rottman Eye Care, our eye care professionals can check for corneal conditions as part of a comprehensive eye exam. Depending on the type and severity of the corneal condition, treatment can range from prescription eye drops, laser treatments, corneal transplants, and scleral lenses for KC patients.
Contact to book an appointment and begin the journey back to clearer vision.